AIM AND PURPOSE
For the past century, diagnosis and treatment of glaucoma has been directed towards increased intraocular pressure (IOP). It is well known that IOP is the most important risk factor associated with the development of glaucoma. New findings, however, show that not all patients with glaucomatous damage have an elevated IOP, and progression of glaucomatous damage may occur even at normal ranges of IOP, including IOP at the lower teens. These observations forced clinicians to take into account other risk factors, besides IOP, which could enhance progression of glaucomatous damage. One such risk factor is the Flammer Syndrome (FS). The relevance of FS for glaucoma will be discussed in this review.
Introduction
Glaucoma is phenomenologically defined as a disease with characteristic loss of retinal ganglion cells and their axons combined with a tissue remodeling of the optic nerve head and of the innermost layer of the retina as well as a change in blood flow. This leads clinically to a visible cupping of the disc and to a measurable thinning of the nerve fiber layer of the retina. Clinically, the patients experience a progressive visual field damage together with a decrease in contrast and color sensitivity. Blood flow reduction, however, can also be observed in the nailfold capillaries of the fingers, indicating that this reduction is not simply due to an increase in IOP or glaucomatous damage. There is a primary component involved. This primary component, as such, is not arteriosclerosis but rather a primary vascular dysregulation (PVD).
A Traditionally, diagnosis and treatment of glaucoma has been directed towards the increased IOP. It is well known that IOP is a most important risk factor.1–3 New findings, however, show that not all patients with glaucomatous damage have an elevated IOP, and progression of GON may occur even at IOP in the low teens.4,5 The basis of these findings was provided by the Swiss scientist Prof. J. Flammer who revolutionized our understanding of the pathogenesis in glaucoma and after whom the Flammer-Syndrome (FS) is named.6,7 This review summarizes the pathogenetic concept of GON by J. Flammer and therapy of glaucoma patients with FS.
PHENOMENOLOGY OF GLAUCOMATOUS OPTIC NEUROPATHY
For the clinician, the most striking difference between GON and other types of optic neuropathies is the optic nerve head (ONH) excavation. There are, however, a number of additional, partially nonspecific, morphological features of GON including8–11:
-
retinal ganglion cell loss
-
optic nerve rim thinning
-
thinning of the retina
-
lateral geniculate nucleus shrinkage
-
cell loss in the visual cortex
-
splinter hemorrhages around the optic nerve
-
activation of glial cells both in the optic nerve head and in the retina
-
peripapillary atrophy
In addition, there are a number of systemic changes leading to the designation of glaucoma.12
RISK FACTORS FOR GLAUCOMATOUS OPTIC NEUROPATHY
As mentioned above, an undisputable risk factor is an increased IOP. But there is evidence in literature that other risk factors are involved as well. These additional factors may by themselves lead to GON or they may render the eye more sensitive to IOP. Among the most often described factors are: increased retinal venous pressure,13 thin cornea14 and low blood pressure particularly in the context of FS.15 In fact, some patients show fluctuations in their visual fields, especially diffuse visual field defects, in response to some environmental changes such as cold hands and this may be explained by changes in ocular blood flow.7,16
Low blood pressure, increased retinal venous pressure and FS are not independent factors as on the one hand, patients with FS often suffer from low blood pressure as well as from increased retinal venous pressure and on the other hand, patients with FS very often have disturbed autoregulation rendering the eye more sensitive to both an increase in IOP and to a decrease in blood pressure. In fact, some studies have found a relationship between FS and normal-tension glaucoma.17,18
BLOOD CIRCULATION
Blood circulation serves as transport of a large variety of molecules including oxygen, cells such as leucocytes and heat. Regulation of blood flow (BF) is necessary to adapt to the varying internal and external conditions. During exercise, for example, the oxygen demand of the muscles increases dramatically. When we move quickly from a warm to a cold environment, our circulation adapts to redistribute body temperature in order to avoid too much heat loss etc.8
The overall BF is regulated by the cardiac output which is mainly controlled by the autonomic nervous system and circulating hormones. The distribution of this cardiac output (minute volume) to the different organs, or part of organs, is regulated by the relative local resistance to flow.
REGULATION OF LOCAL RESISTANCE
All vessels are under control of the vascular endothelial cells (VEC) which release vasoactive molecules.19 The most important molecules are nitric oxide (NO) inducing vasodilation20 and endothelin-1 (ET-1) inducing vasoconstriction. In addition, the vessels of the retina and the optic nerve head are influenced by the activity of the neural and glial cells (so called neurovascular coupling). Due to the blood-retinal barrier, circulating hormones like ET-1 or angiotensin II have no direct access to smooth muscles cells (SMC) and pericytes and therefore have relative little effect on retinal circulation. The situation is different in the choroid which has fenestrated capillaries. Even larger molecules such as hormones escape the vessels and get direct access to SMC. These hormones in the choroid can also diffuse, to some extent, into the ONH.21
INFLUENCE OF CIRCULATING HORMONES
In a number of diseases, like for example multiple sclerosis, endothelin is increased in the circulating blood. This leads to a reduction of choroidal blood flow and to some extent also to a reduction of ocular blood flow (OBF) in the ONH. These diffusing molecules reach the vessels from the outside, thereby, also influencing the blood-brain barrier which in extreme situations is weakened to the extent that it enables even erythrocytes to escape from the vessels. This leads to the so-called splinter hemorrhages at the border of the ONH.20,21
THE EFFECT OF REDUCED OXYGEN SUPPLY
Oxygen is crucial for the survival of tissues but at the same time it is also potentially very toxic.22 Reactive oxidative species (ROS) damage the cell structures. ROS are mainly produced in the mitochondria. ROS-production depends on the local oxygen tension and on electrical potential of the mitochondria. The latter is a function of the proportion of reduced to oxidized redox carrier in the respiratory chain. If oxygen supply is more or less constantly reduced (e.g. in case of an arteriosclerosis), the tissue can adapt to the change. If the oxygen supply is very low, however, tissue infarction may result.20
A reversible short drop of oxygen leads to a preconditioning. By this way, the tissue can tolerate subsequent drops of oxygen better. The preconditioning is partially mediated by ROS. If the drop of oxygen is stronger, ROS-production can exceed the organism’s capacity to cope with free radicals. As a consequence, oxidative stress damages cellular structures. To some extent, these cellular structures can still be repaired. If the induced damage, however, exceeds the repair capacity, a structural damage will remain. After repeated insults, the structural damages sum up leading finally to a clinically detectable disease.8
VASCULAR DYSREGULATION
A distinction has to be made between primary and secondary vascular dysregulation.23 A systemic vascular dysregulation can be secondary (SVD) as for example in multiple sclerosis. The primary vascular dysregulation (PVD) occurs in otherwise healthy subjects, particularly (but not only), in young, slim females. Subjects with PVD have a compromised autoregulation of ocular perfusion explaining their increased risk for glaucoma, particularly for normal-tension glaucoma.24,25 For this reason, FS will be discussed here in some more detail.
FLAMMER SYNDROME
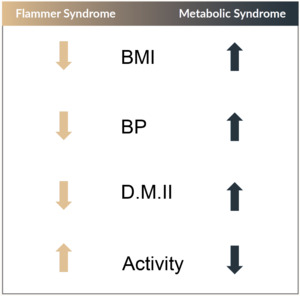
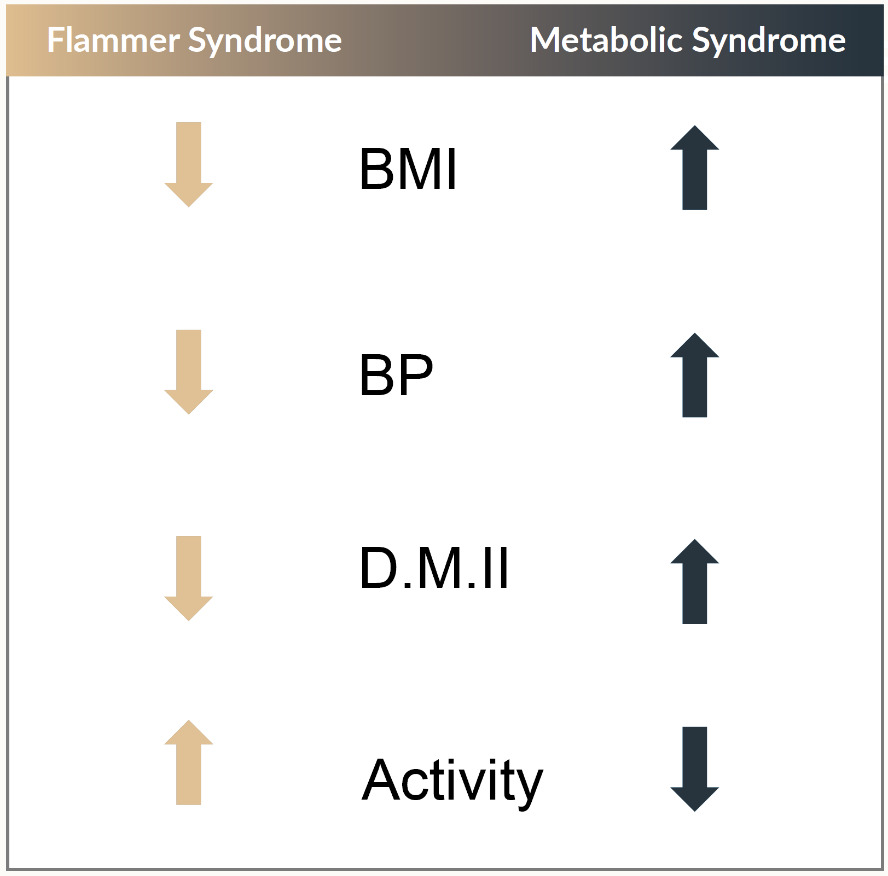
FS is characterized by an inborn tendency to respond differently to a variety of stimuli such as cold, emotional or mechanical stress. The symptoms might already be present in childhood but become clearly manifest during puberty and mitigate as subjects get older, in particular during menopause. The syndrome is observed more often in women than in men, in slim than in obese people (Figure 1), in academics than in blue color workers, in Asians than in Caucasians. The leading symptom in FS is cold hands and feet.26,27 People with FS often state to suffer from cold hands, but when measured, their feet are cold as well.23 The feeling of thirst of people with FS is also reduced.28 They normally drink enough but not because they are thirsty, rather, because they know that they have to drink. People with FS also have a prolonged sleep onset time.29 The reason for this, is that there is a strong connection between feet temperature and sleep onset time. These people have colder feet explaining why they need longer to warm them up. People with FS also have an altered drug sensitivity. This is at least partially due to an altered gene expression of the ATP-binding cassette (ABC) transport proteins.30 Another common symptom of FS is low blood pressure and a higher sensitivity to ET-1 which is blood pressure dependent.31 People with FS also have a better smell perception than others and higher retinal venous pressures leading to an increased risk for retinal vein occlusions.32–35 People with FS have reversible diffuse visual field defects (best represented with the Bebie-curve) and their retinal vessels show a higher spatial irregularity and are stiffer.36–38 The vasodilation to flickering light is reduced in other words, the neurovascular coupling is suppressed.39 Ocular blood flow of FS people is correlated with peripheral blood flow.26 The circulation of their eye is paradoxically related to perfusion pressure meaning that their autoregulation is disturbed.17 This disturbed autoregulation is the major link from FS to GON. For this reason, the pathogenetic concept of GON by J. Flammer will be discussed below.
PATHOGENETIC CONCEPT (BY J. FLAMMER)
Before FS was known, investigators searched for a relationship between glaucomatous damage and atherosclerosis and its risk factors such as smoking, diabetes or arterial hypertension. These results, however, were mostly disappointing.40 Today we know that atherosclerosis and its risk factors indeed also lead to glaucoma but rather via an increased IOP (high-tension glaucoma [HTG]), whereas FS contributes to glaucomatous damage via a disturbed autoregulation of ocular perfusion.17 People with atherosclerosis or its risk factors, on the average, have a higher IOP. This relationship is statistically significant but weak.
In the center of the pathogenetic concept is an unstable blood flow.41,42 Blood flow is either unstable if the IOP fluctuates at a high level (as in HTG) or if IOP and blood pressure fluctuate at a low level (as in normal-tension glaucoma [NTG]), particularly those with FS who commonly have high retinal venous pressures.33 The instability of the blood flow, together with the activation of astrocytes leads to a chronic oxidative stress with ultimately causes cell damage.43,44
THERAPEUTIC CONSEQUENCES
Although many people suffer from a FS, to date, only little is known about treatment. Our recommendations, therefore, rely more on clinical experience than on controlled studies. Moreover, we will focus on the value of non-IOP lowering treatment for glaucoma patients with FS as IOP-lowering treatment strategies have been previously discussed in the literature thoroughly. The therapeutic suggestions made here are also valuable for FS people not suffering from glaucoma.
In a first step, we recommend to improve the bodies overall circulation by proper but not extreme activities. People with FS should refrain from certain activities even when they are beneficial for other individuals, such as prolonged fasting. Some people with FS may respond well to acupuncture and others to sauna baths. In contrast to patients with high blood pressure, people with FS with low blood pressure should have sufficient salt intake and drink enough water, particularly in the evening. In severe cases of low blood pressure, patients may be treated with low doses of fludrocortisone (0.1 mg 2 x a week). Patients suffering from orthostatic hypotension should wear supporting stockings. The intake of magnesium is also beneficial, as magnesium (a physiological calcium channel blocker, CCB) improves vascular regulation. Treatment with CCBs reduces increased retinal venous pressures in glaucoma patients with FS. Healthy people with FS benefit from drinking borage tea, as borage has CCB side effects similar to verapamil and reduces increased retinal venous pressures in people with FS.45 Blood flow regulation may also be improved by carbonic anhydrase inhibitors.46 Omega-3-fatty acids (Omega 3-FA’s) have a number of different effects including the modulation of intracellular calcium ion release and thereby the stabilization of circulation.47 Omega 3-FA’s also increase the production of uncoupling proteins and thereby improve ATP-independent heat production which is most probably impaired in patients with FS.48,49
There is still no answer to the question as to whether estrogen replacement therapy for women after menopause is beneficial. Without doubt, estrogens (female hormones) have some positive effects. Nevertheless, in individuals with FS exacerbation has been observed with estrogen therapy. Therefore, we recommend for post-menopausal female patients having FS to measure ocular blood flow before initiating estrogen therapy and again three months after its introduction. If blood flow stays the same or even improves, the ophthalmologist will not object to long-term estrogen therapy.
As mentioned before, oxidative stress is involved in the pathogenesis of glaucoma.35 The target of oxidative stress relevant in the development of GON are most probably the mitochondria.35,50 It is therefore desirable to have a drug protecting the mitochondria, in particular the mitochondria of the optic nerve head.50 This can unfortunately not be achieved by an increase in intake of vitamins such as vitamin C or vitamin E. Only molecules reaching the inner membrane of the mitochondria can be of potential use. The flavonoids of ginkgo biloba can penetrate the mitochondria to reduce oxidative stress and thereby protect the retinal ganglion cells.51–55 Moreover, ginkgo has been shown to improve visual fields in a long term double masked placebo-controlled study.56 Reports have suggested a daily dose of 120 mg to be sufficient and acceptable.57
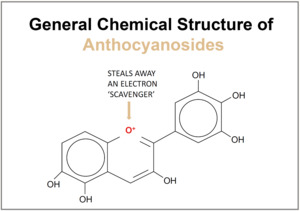
Foods containing polyphenolic flavonoids such as red wine, green tea, dark chocolate or coffee are also potentially beneficial.58,59 Coffee is not only rich in flavonoids but also contains the molecule 3-methyl-1,2-cyclopentanedione (MCP) which has been shown to be a selective scavenger of the peroxynitrite (Figure 2).60 Anthocyanins, rich in foods such as bilberry, are another class of substances with antioxidant properties. In addition to polyphenolic rings, anthocyanins possess a positively charged oxygen atom in their central ring which enables them to readily scavenge electrons (Figure 3).61,62